Movement Difficulties
Damage to the motor fibers interferes with muscle control and can cause weakness, loss of muscle bulk, and loss of dexterity. Sometimes, cramps are a sign of motor nerve involvement.
Other muscle-related symptoms include:
– Lack of muscle control
– Difficulty or inability to move a part of the body (paralysis)
– Muscle atrophy
– Muscle twitching (fasciculation) or cramping
– Difficulty breathing or swallowing
– Falling (from legs buckling or tripping over toes)
– Lack of dexterity (such as being unable to button a shirt)
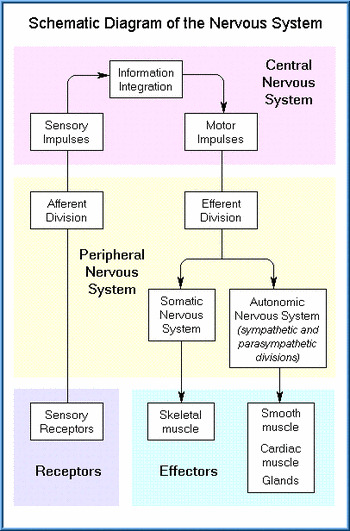
Autonomic Symptoms
The autonomic nerves control involuntary or semi-voluntary functions, such as control of internal organs and blood pressure. Damage to autonomic nerves can cause:
– Blurred vision
– Decreased ability to sweat
– Dizziness that occurs when standing up or fainting associated with a fall in blood pressure
– Heat intolerance with exertion (decreased ability to regulate body temperature)
– Nausea or vomiting after meals
– Abdominal bloating (swelling)
– Feeling full after eating a small amount (early satiety)
– Diarrhea
– Constipation
– Unintentional weight loss (more than 5% of body weight)
– Urinary incontinence
– Feeling of incomplete bladder emptying
– Difficulty beginning to urinate (urinary hesitancy)
– Male impotence
Exams and Tests
A detailed history is needed to determine the cause of the neuropathy. Neurological examination may reveal abnormalities of movement, sensation, or organ function. Changes in reflexes and muscle bulk may also be present. Tests that reveal neuropathy may include:
– EMG (a recording of electrical activity in muscles)
– Nerve conduction tests
– Nerve biopsy
– Blood tests to screen for medical conditions, such as diabetes and vitamin deficiency, among others.
Tests for neuropathy are guided by the suspected cause of the disorder, as suggested by the history, symptoms, and pattern of symptom development. They may include various blood tests, x-rays, scans, or other tests and procedures. Some people are told they have a problem with the myelin sheath that coats the nerves. While this is ‘common sense’ assumption, that diagnosis can only be confirmed via a biopsy (cutting the nerve and removing a portion of it), which destroys the nerve. You have to be careful not to accept the common catch-all explanation of the cause of your neuropathy being from damage to the myelin sheath. If your physician did not surgically remove a section of your nerve and send it to a lab for analysis, then the actual condition of your myelin sheath is unknown and probably just a guess.
References:
Delalande S, de Seze J, Fauchais AL, et al. Neurologic manifestations in primary Sjogren syndrome: a study of 82 patients. Medicine (Baltimore). 2004 Sep;83(5):280-91.
Mori K, Iijima M, Sugiura M. Sjogren’s syndrome associated painful sensory neuropathy without sensory ataxia. J Neurol Neurosurg Psychiatry . 2003 Sep;74(9):1320-2.

Contact Us
Newsletter
Quick Links
Contact Info
Frequency Rising
13239 Sundance Ave. San Diego, CA 92129
800-701-4039 9am – 5pm PST
info@peripheralneuropathytreatments.com